by Sharon Begley
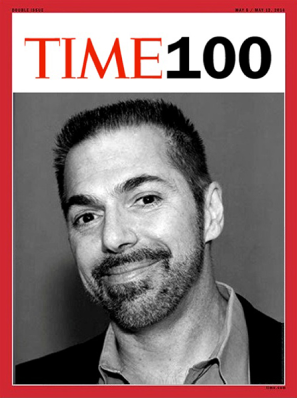
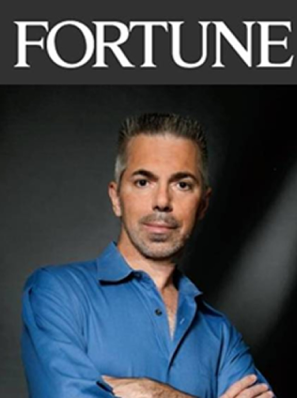
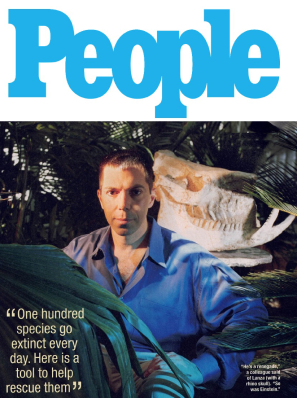
Embryonic” and “senescent” aren’t supposed to go together any more than “good” and “grief” or other oxymorons, which is why biologist Robert Lanza was “devastated” when he saw what was happening with the human stem cells he and colleagues were trying to grow. Like hundreds of other stem-cell scientists, they had been intrigued…
BY SHARON BEGLEY
Embryonic” and “senescent” aren’t supposed to go together any more than “good” and “grief” or other oxymorons, which is why biologist Robert Lanza was “devastated” when he saw what was happening with the human stem cells he and colleagues were trying to grow. Like hundreds of other stem-cell scientists, they had been intrigued and energized by the 2007 discovery that adult cells can be regressed back to an embryonic state simply by inserting four genes into them. The discovery, by scientists at Kyoto University and the University of Wisconsin-Madison, seemed to promise a way out of the bitter debates over embryonic-stem-cell research: rather than using human embryos as a source of stem cells, produce them from adult cells.
Like cells from days-old embryos, the resulting induced pluripotent stem (iPS) cells have the ability to differentiate into any of 220 kinds of human cells, from neurons to retinal cells to pancreatic cells. Their promise was so great that when President Obama announced last March that he was lifting the ban on the use of federal money for research on human embryonic stem cells, critics on the right were apoplectic: iPS cells, they said, made such a move scientifically unjustified. Even President George W. Bush’s bioethics council cited the promise of iPS cells in chastising Obama).
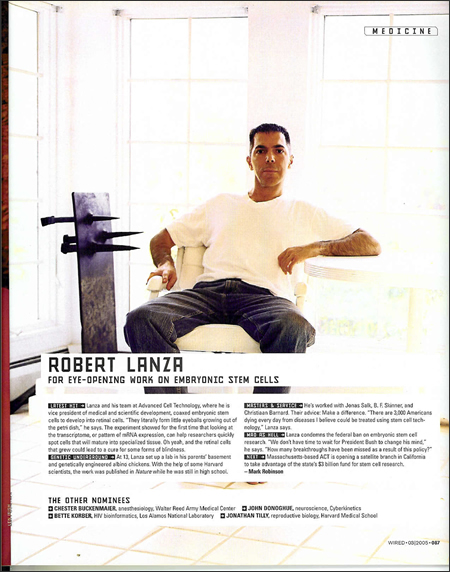
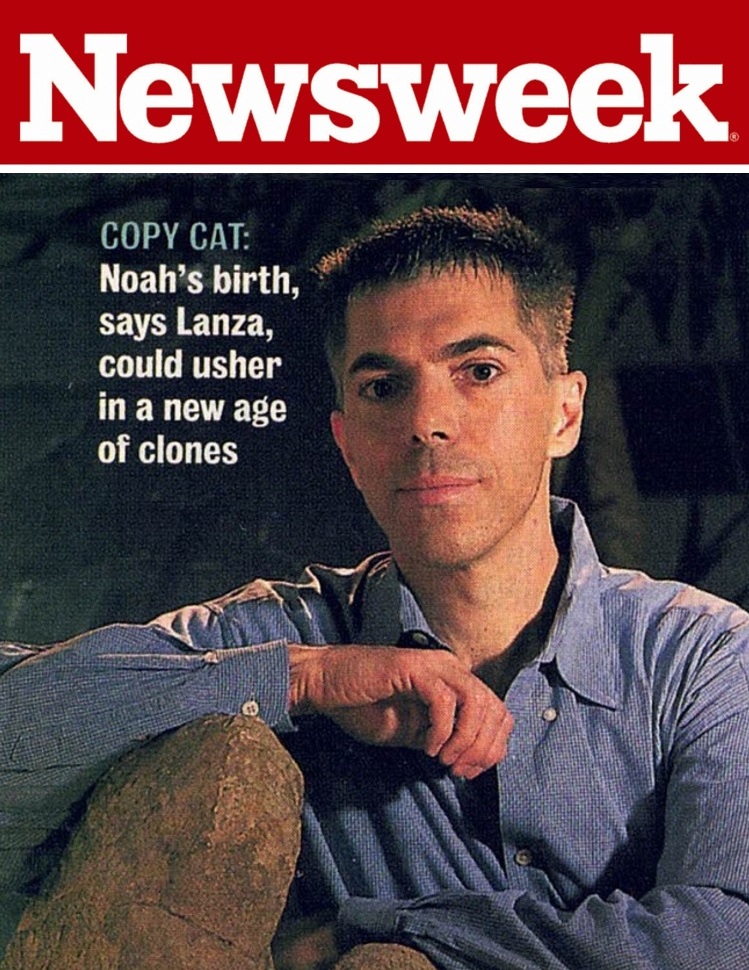
Lanza, the chief scientific officer at Advanced Cell Technology, and colleagues shared the optimism about iPS cells. They were trying to grow various types of cells from the iPS cells. It went fine at first, with the iPS cells differentiating into blood, vascular, and retinal cells as intended, the scientists are reporting today in the journal Stem Cells. But things went south fast. Compared with specialized cells produced from the 25 lines of stem cells derived from embryos, those from the eight populations of iPS cells in the study had significantly higher rates of death through a mechanism called apoptosis (which is basically a suicide program within the cells), higher rates of aging (senescence), and severely lower rates of growth. The retinal cells and blood-vessel cells in particular were about as sprightly as cells ready for a nursing home, and lost their crucial ability to continue dividing.
“We just couldn’t get the cells to do what we wanted,” Lanza told me. “At first we blamed ourselves, but then we looked at the cell markers and saw that the cells were aging much faster” than true embryonic cells. “There was a 1,000- to 5,000-fold difference” between the iPS cells’ ability to keep growing and dividing and the true embryonic cells’ ability, he says. “In terms of whether you can use the cells therapeutically or to study disease, that’s the difference between getting the study to work and being dead in the water.” Other scientists working with iPS cells have begun to see the same problems, Lanza says, suggesting that “this whole population of cells is screwed up.”
That is bad news for both of the hoped-for uses of iPS cells. The first is therapy, such as transplanting neurons into the brain of Parkinson’s patients or retinal cells into the blind. Obviously, transplanting cells that will age and die prematurely has failure written all over it. The second use is in understanding the cause and trajectory of disease: studying stem cells from patients with, say, diabetes or Alzheimer’s to see exactly where things go wrong may prove disastrously misleading if the stem cells are fated to age prematurely. Lanza says, “You would have no way of telling whether the problems you were seeing were due to the disease or to these properties of iPS cells.”
All hope is not lost when it comes to iPS cells, however. Lanza suspects that the premature aging may be related to using viruses to carry the turn-back-the-calendar genes into adult cells, which is what “induces” them to act (sort of) like embryonic cells. “It seems pretty clear that you can’t just chop up DNA with viruses and insert new genes without consequences,” Lanza says. But preliminary results suggest that iPS cells produced without viruses or genetic manipulation show less premature senescence. Tissue engineer Anthony Atala, director of Wake Forest University Baptist Medical Center’s Institute for Regenerative Medicine, told Scientific American that the problems Lanza is reporting with iPS cells may therefore be “solvable.”
From his lips to the bioscience gods’ ears. Until then, however, “although there is excitement that iPS cells can serve as an embryo-free source of stem cells,” says Lanza, “it would be premature to abandon research using embryonic stem cells until we fully understand what’s causing these problems.” The fight goes on.