Wall Street Journal
A Massachusetts biotechnology company said it expects as early as Friday to start the process for regulatory approval of what would be the first human trial involving stem cells created by reprogramming adult cells back to an embryonic-like state.
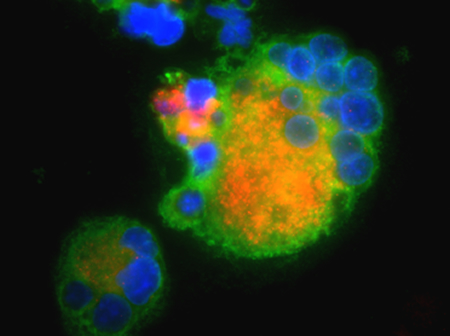
Researchers have been experimenting with treatments derived from stem cells, which can grow into other cell types or tissues. But such cells are typically obtained by destroying human embryos, a controversial practice. Scientists are experimenting with other types of stem cells derived from bone marrow or umbilical cord blood, but such cells are limited in the types of cells they can grow into.
The newer approach involves reprogramming mature cells, typically from the skin, without the need to destroy embryos. Two of the researchers who developed the process shared a Nobel Prize this year for the work.
Advanced Cell Technology Inc. of Marlborough, Mass., says it wants to test blood-clotting particles, called platelets, made from such reprogrammed cells. People with certain forms of leukemia, anemia and other conditions need repeat infusions of platelets to avoid bleeding to death, but can develop resistance to the donated cells over time, making them less effective, experts say. Stem-cell derived platelets could overcome that problem because they could be derived from a patient’s own cells.
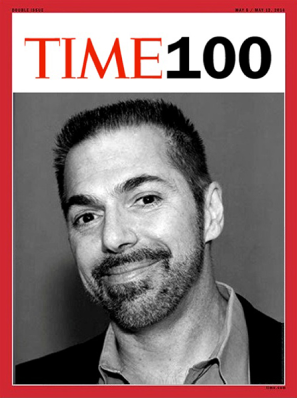
“This would really be a dramatic advance in medicine, but it remains to be seen if this would be successful,” said Alan Michelson, a platelet researcher at Harvard Medical School and Boston Children’s Hospital who would lead a clinical trial in the U.S. studying ACT’s stem-cell derived platelets.
ACT has proposals for clinical trials and says testing could begin as early as the end of next year if regulators sign off. The U.S. Food and Drug Administration declined to comment, saying federal rules prevent it from discussing any therapies that may be under development.
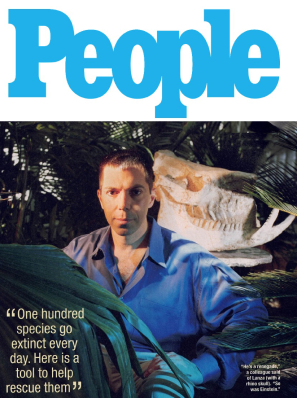
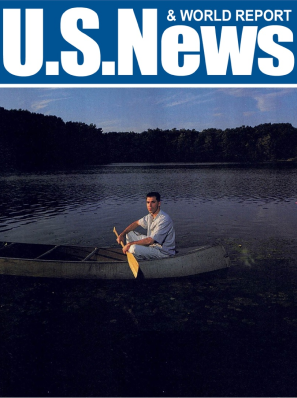
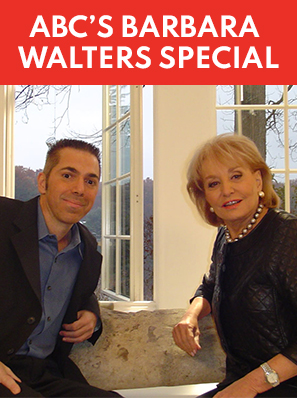
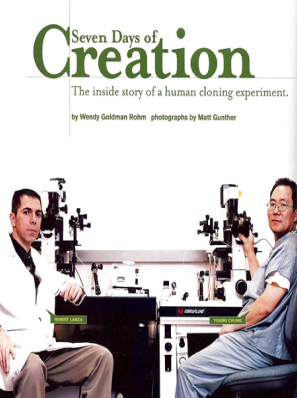
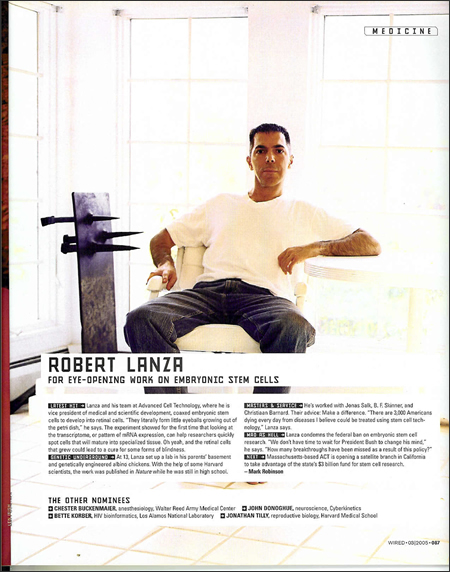
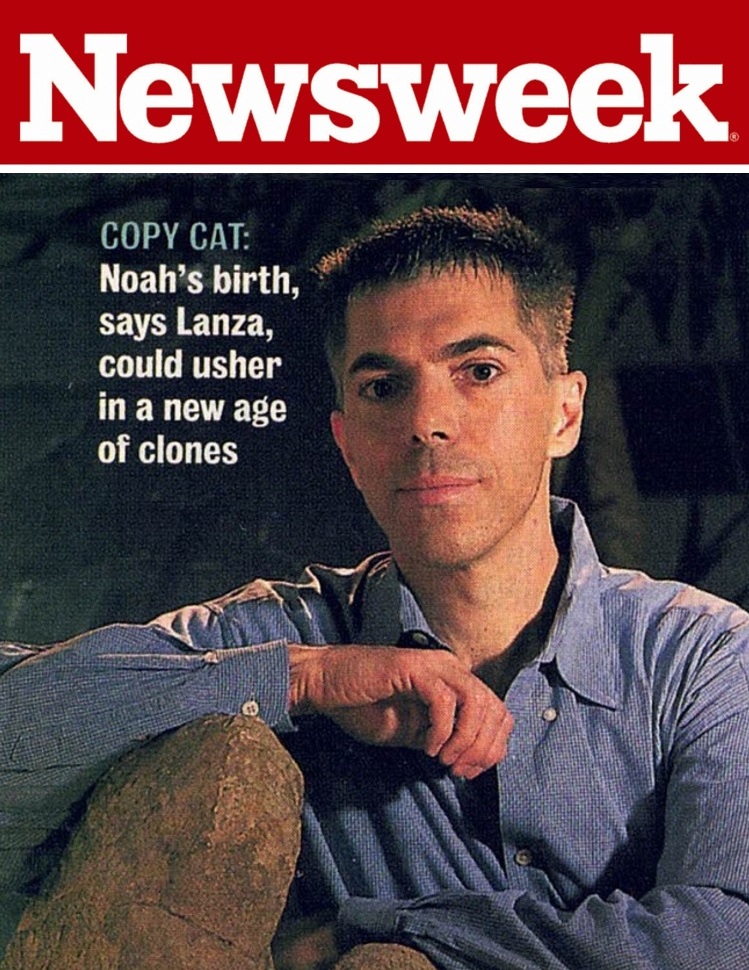
Robert Lanza, ACT’s chief scientific officer, said that the company has the “capacity to make enough” platelets for the initial clinical trials but would “take time to scale up for widespread use.”
“It doesn’t require any embryos. It doesn’t require eggs. It doesn’t require any destruction of embryos,” Dr. Lanza said.
Among the challenges facing laboratories and firms that have been racing to make so-called induced-pluripotent-stem-cell treatments is making enough of the cells. Another is preventing genetic abnormalities to some cells that could cause tumors.
Platelets don’t carry the risk of genetic defects because they don’t have DNA, experts say. Yet a risk remains that some stray cells with DNA could contaminate a batch of the stem-cell derived platelets, according to James Thomson, one of the researchers who first turned human skin cells into pluripotent stem cells in 2007.
“You have to manipulate the cells quite a bit, so I think you’ll have to overcome the safety concerns of the FDA and other regulatory bodies,” said Dr. Thomson, of the Morgridge Institute for Research in Madison, Wis.
Dr. Lanza said ACT takes “multiple measures” to prevent contamination of its supply, and platelets can be irradiated before use.
ACT’s idea for the U.S. trial would be to infuse both normal platelets and stem-cell-derived platelets into eight patients, Dr. Lanza said, and compare how the cells function. A separate set of eight patients would receive normal platelets and platelets derived from human embryonic stem cells.
Each of the cells would be tagged with a chemical allowing researchers to track their presence in study subjects. Researchers would periodically draw blood from study subjects and then analyze the blood to see if the tagged stem-cell-derived platelets are surviving and circulating like normal platelets.
If the stem-cell derived platelets worked like normal platelets, “the potential impact would be great,” said Cynthia Dunbar, a stem-cell researcher at the National Heart, Lung and Blood Institute and editor of the journal Blood.
Link to article on Wall Street Journal